Craniofacial, Unilateral Cleft Lip Repair cleft lip repair,cleft,lip,plastic,repair,cleft lip,cleft,lip,repair cleft lip,plastic repair,cleft lip,cleft,cleft,unilateral,cleft,bilateral,cleft lip,repair,cleft,lipBackgroundThe
presence of unilateral cleft lip is one of the most common congenital
deformities. A broad spectrum of variations in clinical presentation
exists. Unilateral cleft lip involves deformity of the lip in addition
to the alveolus and nose. Patients with this deformity require
short-term care and long-term care and follow-up from practitioners in
multiple specialties.
[1] Patients
may need multiple surgical interventions, from infancy to adulthood, in
order to achieve necessary function and aesthetic quality. No
universal agreement has been reached as to the timing and technique of
repair. Several methods are used with comparable long-term results,
which serves as an indication that more than one treatment option exists
for definitive repair. Treatment goals include the restoration of
facial appearance and oral function, improvement of dental skeletal and
occlusal relationships, improvement of speech, and the psychosocial
state.
Next Section: History of the Procedure
History of the ProcedureIn
1843, closure of the unilateral cleft lip with local flaps was
described by Malgaigne. The following year, Mirault modified Malgaigne’s
technique by using the lateral lip flap to fill the medial defect. All
future methods of cleft lip closure are based on Mirault’s technique.
LeMesurier and Tennyson modified this technique with a quadrilateral and
triangular flap, respectively. In 1976, Millard published his
definitive repair in which the lateral flap advancement into the upper
portion of lip was combined with downward rotation of medial lip.
[2] Other modifications have been published by Noordhoff, Mohler, and Onizuka.
[3, 4] Fisher
has described an anatomical subunit approximation for definitive cleft
lip repair. Millard’s methods, including variations, remain among the
most popular method for unilateral cleft lip closure.
[4] Cleft
lip surgery has evolved from a simple adhesion of paired margins of the
cleft to an understanding of the various malpositioned elements of the
lip to a more complicated geometric reconstruction using transposition,
rotation, and advancement flaps.
[5] Previous
Next Section: History of the Procedure
ProblemThe
cleft affects the facial form as an anatomic deformity and has
functional consequences. These include the child's ability to eat,
speak, hear, and breathe. Consequently, rehabilitation of a child born
with a facial cleft must involve a multidisciplinary approach and staged
appropriately with the child's development, balancing the timing of
intervention against its effect on subsequent normal growth.
Previous
Next Section: History of the Procedure
Epidemiology
FrequencyThe
overall occurrence of cleft lip with or without cleft palate is
approximately 1 in 750-1000 live births. Racial differences exist, with
the incidence in Asians (1:500) greater than in Caucasians (1:750)
greater than in African Americans (1:2000). The incidence of cleft
lip/palate is more common in males.The most common presentation is cleft lip and palate (approximately 45%), followed by cleft palate alone (35%) and cleft lip alone (approximately 20%). Unilateral cleft lips are more common than bilateral cleft lips and occur more commonly on the left side (left cleft lip:right cleft lip:bilateral cleft lip = 6:3:1).The
risk of a newborn having a cleft lip increases if a first-degree
relative also has a cleft. If one child already has a cleft lip, the
chance of a second child being born with the deformity is 4%. If a
parent has a cleft lip, the chance of a newborn having a cleft is 7%. If
both a parent and a sibling have a cleft lip, the newborn's risk rises
to 15%.
Previous
Next Section: History of the Procedure
EtiologyClefting has a multifactorial basis, with both genetic and environmental causes
cited. The observation of clustered cases of facial clefts in a
particular family indicates a genetic basis. Clefting of the lip and/or
palate is associated with more than 150 syndromes. The overall incidence
of associated anomalies (eg, cardiac) is approximately 30% (more common
with isolated cleft palate).Environmental causes, such as viral infection (eg, rubella)
and teratogens (eg, steroids, anticonvulsants), during the first
trimester have been linked to facial clefts. The risk also increases
with parental age, especially when older than 30 years, with the
father's age appearing to be a more significant factor than the mother's
age. Nevertheless, most presentations are of isolated patients within
the family without an obvious etiology.Midfacial development
involves several sets of genes, including those involved in cell
patterning, proliferation, and signaling. Mutations in any of these
genes can change the developmental process and contribute to cleft
development. Some of these genes include the
DIX gene, sonic hedgehog (
SHH) gene, transforming growth factor (
TGF) alpha/beta, and interferon regulatory factor (
IRF6).
Classification
Kernahan developed a classification scheme in which the defect can be classified
onto a Y-shaped symbol. In this diagram, the incisive foramen is
represented as the focal point. This system has been applied to both
cleft lip and palate
.

Millard
modification of Kernahan striped-Y classification for cleft lip and
palate. The small circle indicates the incisive foramen; the triangles
indicate the nasal tip and nasal floor.
Previous
Next Section: History of the Procedure
PathophysiologyWhile the normal embryologic development of the face is detailed in Head and Neck Embryology, a brief outline relevant to the formation of facial clefts follows.In
short, the branchial arches are responsible for the formation of
several areas, including the mouth and lip. Mesenchymal migration and
fusion occurs during weeks 4-7 of gestation. The first branchial arch is
responsible for the formation of the maxillary and mandibular
processes. The maxillary and mandibular prominences form the lateral
borders of the primitive mouth or stomodeum.Mesenchymal migration
and fusion of the primitive somite-derived facial elements (central
frontonasal, 2 lateral maxillary, mandibular processes), at 4-7 weeks
gestation, is necessary for the normal development of embryonic facial
structures. When migration and fusion are interrupted for any reason, a
facial cleft develops along embryonic fusion lines. The embryonic
development of the primary palate (lip and palate anterior to the
incisive foramen) differs from the secondary palate (palate posterior to
the incisive foramen).The developing processes of the medial
nasal prominence, lateral nasal prominence, and maxillary prominences
form the primary palate. Fusion occurs, followed by "streaming" of
mesodermal elements derived from the neural crest. In contrast, the
secondary palate is formed by the fusion of palatal processes of the
maxillary prominence alone. The difference in embryonic development
suggests the possibility of differing degrees of susceptibility to
genetic and environmental influences and accounts for the observed
variation in incidences.In summary, unilateral cleft lip results from failure of fusion of the medial nasal prominence with the maxillary prominence.
Previous
Next Section: History of the Procedure
PresentationFor
treatment purposes, unilateral cleft lip can be placed into one of
three categories: microform/forme fruste, incomplete, or complete cleft
lip.
- Microform cleft (forme fruste):
This defect is characterized by a "light" furrow along the vertical
length of the lip with a small vermilion notch and minor imperfections
in the white roll. A small component of vertical lip length deficiency
and associated nasal deformity may be present.
- Incomplete
cleft lip: This defect is characterized by the varying degree of
vertical lip separation. By definition, it has an intact nasal sill,
commonly termed the Simonart band.
- Complete
cleft lip: This involves the full-thickness defect of the lip and
alveolus (primary palate), extends into the base of the nose (no
Simonart band exists), and is often accompanied by a palatal cleft
(secondary palate). The premaxilla is typically rotated outward and
projects anteriorly in relation to a relatively retropositioned lateral
maxillary alveolar element.
As a consequence of the
clefting of the lip, an associated nasal deformity occurs. The
structures of the ala base, nasal sill, vomer, and septum are distorted
significantly. The lower lateral cartilage on the cleft side is
positioned inferiorly, with an obtuse angle as it flattens across the
cleft. The alar base is rotated outward. The developing nasal septum
pulls the premaxilla away from the cleft, and the septum and the nasal
spine are deflected toward the noncleft side. The cleft may continue
through the maxillary alveolus and palatal shelf, extending to the
palatal bone and soft palate.
Further treatment planningOrthodontic treatment can be initiated a few weeks following birth, prior to
surgical intervention. Other adjunct procedures include lip adhesion,
presurgical orthopedics, primary nasal correction, and nasoalveolar
molding. These procedures attempt to reduce the deformity. Nasoalveolar
molding is the active molding and repositioning of the nasal cartilage
and alveolar processes with an appliance.
[6] This
orthodontic intervention takes advantage of the plasticity of the
cartilage. Presurgical nasal alveolar allows repositioning of the
maxillary alveolus and surrounding soft tissues in hopes of reducing
wound tension and improving results.
[7, 8] Definitive
repair is delayed until approximately 3 months of age; this varies,
depending on physician comfort. A multidisciplinary approach should be
carried out over several years for patients with unilateral cleft lip.
This team should include practitioners from audiology, otolaryngology,
and speech therapy, among other specialities.
Previous
Next Section: History of the Procedure
IndicationsPatients
born with a cleft lip should undergo surgical repair unless otherwise
contraindicated. The goal of reconstruction is to establish normal
morphologic facial form and function in order to provide the optimal
conditions for the development of dentition, mastication, hearing,
speech, and breathing, and psychosocial status.
Previous
Next Section: History of the Procedure
Relevant AnatomyNormal
lip and nasal anatomy is essential for an understanding of the
distortion caused by a facial cleft. The elements of the normal lip are
composed of the central philtrum, demarcated laterally by the philtral
columns and inferiorly by the Cupid's bow and tubercle. Just above the
junction of the vermilion-cutaneous border is a mucocutaneous ridge
frequently referred to as the white roll. Within the red vermilion of
the lip is a noticeable junction demarcating the dry and wet vermilion,
the increased keratinized portion of the lip that is exposed to air from
the moist environment of the labial mucosa. The primary muscle
of the lip is the orbicularis oris, and it has two well-defined
components: the deep (internal) and the superficial (external)
components. The deep (internal) fibers run horizontally or
circumferentially from commissure (modiolus) to commissure (modiolus)
and functions as the primary sphincteric action for oral feeding. The
superficial (external) fibers run obliquely, interdigitating with the
other muscles of facial expression to terminate in the dermis. They
provide subtle shades of expression and precise movements of the lip for
speech. The superficial fibers of the orbicularis decussate in
the midline and insert into the skin lateral to the opposite philtral
groove forming the philtral columns. The resulting philtral dimple
centrally is depressed as there are no muscle fibers that directly
insert into the dermis in the midline. The tubercle of the lip is shaped
by the pars marginalis, the portion of the orbicularis along the
vermilion forming the tubercle of the lip with eversion of the muscle. In
the upper lip, the levator labii superioris contributes to the form of
the lip. Its fibers, arising from the medial aspect of the infraorbital
rim, sweep down to insert near the vermilion cutaneous junction. The
medial-most fibers of the levator labii superioris sweep down to insert
near the corner of the ipsilateral philtral column and
vermilion-cutaneous junction, helping to define the lower philtral
column and the peak of the Cupid's bow. The nasal muscles are
equally important. The levator superioris alaeque arises along the
frontal process of the maxilla and courses inferiorly to insert on the
mucosal surface of the lip and ala. The transverse nasalis arises along
the nasal dorsum and sweeps around the ala to insert along the nasal
sill from lateral to medial into the incisal crest and anterior nasal
spine. These fibers join with the oblique fibers of the orbicularis and
the depressor septi (nasalis), which arises from the alveolus between
the central and lateral incisors to insert into the skin of the
columellar to the nasal tip and the footplates of the medial crura. A
unilateral cleft thus disrupts the normal termination of the muscle
fibers that cross the embryologic fault line of the maxillary and nasal
processes, resulting in symmetric but abnormal muscular forces between
the normal equilibrium that exists with the nasolabial and oral groups
of muscles. With an unrestrained premaxilla, the deformity accentuates
with differential growth of the various elements. The alar cartilages
are splayed apart and rotate caudally, subluxed from the normal
position. Consequently, the nasal tip broadens, the columellar is
foreshortened, and the alar bases rotate outwardly cephalad.
Previous
Next Section: History of the Procedure
Contraindications
- Malnutrition,
anemia, or other pediatric conditions that result in the patient's
inability to tolerate general anesthesia are contraindications to this
procedure.
- Cardiac anomalies that may coexist must be addressed prior to the lip repair
Craniofacial, Unilateral Cleft Lip Repair WorkupLaboratory Studies
- Perform
a thorough physical examination, not limited to the head and neck
region, to uncover associated anomalies in the infant presenting with a
unilateral cleft lip with or without a palatal cleft. Additional workup
is determined by physical findings that suggest involvement of other
organ systems.
- The child's weight, oral intake, and growth and/or development are of primary concern and must be followed closely.
- Routine laboratory studies typically are not required, other than a hemoglobin study shortly before the planned lip repair.
- Routine imaging is not indicated in a healthy patient with isolated cleft lip.
- Craniofacial, Unilateral Cleft Lip Repair Treatment & Management
- Surgical Therapy
Children
born with a facial cleft benefit from multidisciplinary clinical care.
This is a team-based approach allowing efficient coordination of all
aspects of care. Beyond the lip repair are other issues such as hearing,
speech, dental, and psychosocial integration. With the
multidisciplinary approach, as the child grows, comprehensive care can
be given from birth through adolescence. These associated issues are as
important as the anatomic reconstruction, and ultimately the functional
outcome of the reconstruction depends on addressing them. Each
specialty involved must evaluate the child individually and formulate a
treatment plan, then the team forms a combined individual integrated
protocol that follows the Parameters of Care Guidelines established by
the American Cleft Palate Craniofacial Association. Rather than strictly
adhering to any one protocol, each child is assessed based on the
present need in his or her development, and a treatment plan is created
based on the team's experience.
Next Section: Preoperative Details
Preoperative Details
While
the lip repair is the initial focus for many parents, treatment begins
by assessing the child's nutritional status and assisting the parents
with oral feeding techniques so that appropriate weight gain occurs. Parents
who suddenly are faced with caring for a child with a facial cleft are
overwhelmed. The importance of spending sufficient time with them to
allay their fears, to discuss staging and timing of reconstruction, to
stress the need for involvement of other specialists, and to instruct
them on the importance of long-term and consistent follow-up care from
birth through adolescence cannot be overemphasized. The optimal
timing of the surgical repair is still somewhat controversial. Some
centers have advocated surgery in the early neonatal period, with a
theoretical benefit in the scar appearance and nasal cartilage
adaptability, thus minimizing the nasal deformity. To minimize
anesthetic risks, some still adhere to the rule of 10s: perform surgical
repair of cleft lip when the child has a hemoglobin of 10 g, weight of
10 lb, and is aged 10 weeks. In general, however, most centers prefer to
perform the unilateral lip repair when the infant is aged 2-4 months;
anesthesia risks are lower, the child is better able to withstand the
stress of surgery, and lip elements are larger and allow for a
meticulous reconstruction. Before the definitive lip surgery,
cleft centers utilize lip taping, alone or in combination with a passive
intraoral appliance or an active pin-based appliance (eg, Latham) to
align the maxillary arch segments; or no presurgical orthopedic
intervention at all. This choice depends on the center's protocol and
resources. A number of cleft centers prefer to use a passive
intraoral orthodontic palatal appliance to maintain the arch width to
prevent the nearly inevitable collapse that occurs with the lip surgery.[6] The
lip repair reestablishes the soft tissue and muscular forces on the
easily moldable maxillary arch segments. Additionally, this appliance
may include a nasal extension to help improve the nasal tip form. This
nasal alveolar molding device is incorporated into the intraoral
appliance. Several weeks of treatment prior to the surgery and regular
adjustments are needed to mold the alar cartilages into a more favorable
position, thus facilitating the surgical correction of the nasal
deformity. Impressions are taken soon after birth so that the custom
appliance can be applied as soon as possible before the lip repair. The
appliance also assists in the child's oral feeding, helping to decrease
nasal regurgitation and assisting oral suction.
Previous
Next Section: Preoperative Details
Intraoperative Details
The
ideal lip repair results in symmetrically shaped nostrils, nasal sill,
and alar bases; a well-defined philtral dimple and columns; and a
natural appearing Cupid's bow with a pout to the vermilion tubercle. In
addition, it results in a functional muscle repair that with animation
mimics a normal lip. While ideally the lip scars approximate natural
landmarks, ultimately the eye first focuses on symmetry and then normal
contours of the lip at rest and in animation. A number of
surgical procedures for the repair of a unilateral cleft lip are well
described, with a multitude of variations, including the LeMesurier
quadrilateral flap repair, Randall-Tennison triangular flap repair,
Millard rotation-advancement repair,[9] and
Skoog and Kernahan-Bauer upper and lower lip Z-plasty repairs. Many
other variations exist; of particular note are the repairs by Delaire
and by Poole
- .

- The Rose-Thompson repair involves curved or angled paring of the cleft margins to lengthen the lip as a straight-line closure.
 Hagedorn-LeMesurier
Hagedorn-LeMesurier
repair. The medial lip element is lengthened by introducing a
quadrilateral flap developed from the lateral lip
- element.
-

- Tennison-Randall
repair. The medial lip element is lengthened by introducing a
triangular flap from the inferior portion of the lateral
- lip element.
-

- Skoog
repair. The medial lip element is lengthened by introducing two small
triangular flaps developed from the lateral lip element. Each
of these techniques ultimately has the common goal of achieving
symmetry and restoring the continuity of the underlying orbicularis
muscle. All attempt to lengthen the foreshortened philtrum on the cleft
side by interposing tissue from the lateral lip element into the medial
lip element through various combinations of rotation, advancement, and
transposition flaps. While none of the repairs is ideal, each has
advantages and disadvantages, and each results in an excellent repair
in experienced hands, underscoring the fact that more than a single
acceptable technique, rather than a single ideal repair, is available.
However, because of the limitations of this article, the authors choose
to focus on the repair Millard first described in 1955, as today it is
perhaps the most commonly adapted repair of cleft lip. The
rotation-advancement method of Millard advances a mucocutaneous flap
from the lateral lip element into the gap of the upper portion of the
lip resulting from the inferior downward rotation of the medial lip
element.[9] The
repair attempts to place the lip scars along anatomic lines of the
philtral column and nasal sill. Conceptually, Millard's approach is
elegant but it is not always technically easy to accomplish without some
modifications to deal with the wide variation in clefts. As with any
other repair, consistency in achieving a good result is
operator-dependent. A cursory description of a modified Millard operative technique used by the authors is as follows:
- Use
general anesthesia with a noncuffed oro-Rae endotracheal tube
positioned midline. Typically the otolaryngologist then examines the
ears; if needed, myringotomy and pressure equalizing tubes are placed.
- Prior
to infiltration with a local anesthetic (0.5% lidocaine with 1:200,000
epinephrine), mark the anatomic landmarks and tattoo them with a
methylene blue dye.
-
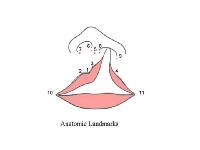
- Figure
illustrates important anatomic landmarks used in all cleft lip repairs.
Measurements of various distances are used to guide the surgeon in
creating a symmetric lip.
- Two
key elements are involved in the markings: the placement of the final
position of the new Cupid's bow peak and the vertical length of the
philtral column to be created on the cleft side. Referring to the
diagram, Point 3 is determined as the mirror image of Point 2 based on
the distance from the midpoint to the peak of the Cupid's bow on the
noncleft side. The peak on the cleft side, Point 4, is not determined as
easily but typically is placed level with Point 2, where the dry
vermilion is widest and the white roll above is well developed. The
white roll and dry vermilion taper off medial to this point. It is
unreliable to determine the peak on the cleft side using the distance
between the peak of the Cupid's bow from the commissure on the noncleft
side because of unequal tension of the underlying orbicularis muscle.
- Once
the anatomic points are marked, draw incision lines that define the 5
flaps involved in the lip reconstruction. These are the inferior
rotation flap (R) of the medial lip element, the medial advancement flap
(A) of the lateral lip element, the columellar base flap (C) of the
medial lip element, and the two pared mucosal flaps of the medial (m)
and lateral (l) lip elements. Two additional flaps that refine the
repair often are used: a white roll flap and a vermilion triangular flap
to allow for a smoother transition at the vermilion cutaneous junction
and at the vermilion contour.
- The
essential marking is the line that determines the border between the R
and C flaps. This line becomes the new philtral column on the cleft
side. For the vertical lengths of the philtrum on the cleft side and
noncleft side to be symmetric, the length of the rotation advancement
flap (y) should equal the vertical length of the philtral column (x) on
the noncleft side (distance between alar base and Cupid's bow peak). For
the two lengths, x and y, to be equal, the path of y must be curved as
illustrated. In marking the curve, take care to avoid a high arching
curve that comes too high at the columellar base to create a generous
philtrum, as this significantly diminishes the size of the C flap.
- While
all flaps are marked, the authors typically refine the design of the A
flap after the R and C flaps are repositioned appropriately so that it
more accurately is tailored to fill the gap left by the inferior
rotation of the R flap and the final placement of the C flap.
- Pare
the margins of the cleft and develop the m and l flaps. The l flap can
be used to inset into the nasal vestibule lining, and the m flap can be
used as part of the orolabial vestibule lining as needed. Alternatively,
both flaps can be used to reconstruct the nasal and orovestibular
lining of the nasal floor depending on the situation. The pars
marginalis of the orbicularis typically is tethered by its abnormal
insertion and further is pared, allowing the constricted muscle to
expand.
- In the region of the
vermilion-cutaneous junction, incise the muscle for approximately 2-3 mm
on either side of the cleft paralleling the vermilion border to allow
development of vermilion-cutaneous muscular flaps for final alignment.
- Develop
the R and C flaps by incising the line (x) between the flaps to allow
inferior rotation of the R flap so that it lies horizontally tension
free with Point 3, level with Point 2. For this to occur, release must
be at all levels (skin, subcutaneous tissue, muscle, fibrous attachments
to the anterior nasal spine, labial mucosa). Occasionally an additional
1- to 2-mm back cut just medial to the noncleft philtral column is
required along with a mucosal back cut to allow for adequate inferior
rotation of the R flap. The back cut occasionally can be limited to the
subdermal portion to avoid lengthening the
- cutaneous scar.
-

- Millard
repair. With maximal rotation of the R flap, any residual lip length
discrepancy can be corrected with an inferior Z-plasty or a triangular
flap. In a secondary correction, further rotation of the R flap can be
considered.
- Correspondingly
free the C flap with the medial crus of the alar cartilage and allow it
to be repositioned, creating a large gap to be filled by the A flap.
- Develop
the A flap from the lateral lip element for advancement into the gap
between the R and C flaps. In developing the A flap, keep the incision
along the alar base at a minimum; it rarely is required to extend much
beyond the medial-most aspect of the alar base. The key to allowing
adequate mobilization of the A flap is the subcutaneous release of the
fibrous attachments of the alar base to the piriform margin of the
maxilla and not necessarily a continued cutaneous incision along the
alar margin. Other surgeons have chosen to mobilize the ala at the
subperiosteal level.
-

- Millard
repair. The medial lip element [R] is rotated inferiorly and the
lateral lip element [A] is advanced into the resulting upper lip defect.
The columellar flap [C] is then used to create the nasal sill (see text
for details).
- A
lateral labial mucosal vestibular release also is required to mobilize
the A flap medially and to avoid a tight-appearing postoperative upper
lip deformity. Do not forget that the maxillary alveolar arches
typically are at different heights in the coronal plane, and the ala
must be released completely and mobilized superior medially to achieve
symmetry, although ultimately its maxillary support is inadequate until
arch alignment and bone grafting can be accomplished.
- As
part of the mobilization of the ala, make an incision along the nasal
skin-mucosal vestibular junction (infracartilaginous) where the
previously developed l flap may be interposed if needed. Currently, the
trend is toward more aggressive mobilization and repositioning of the
lower lateral cartilages as an integral part of the cleft lip repair.
- Widely
undermine the nasal tip between the cartilage and the overlying skin
approaching laterally from the alar base and medially from the
columellar base.
- While the A flap
can be inserted as a mucocutaneous flap incorporating the orbicularis,
the authors repair the muscle separately to allow for differential
re-orientation of its vectors. Dissect the muscle from the overlying
skin and the underlying mucosa to accomplish this and divide it into
bundles that can be repositioned and interposed appropriately.
- Once
all the flaps are developed and the medial and lateral lip elements are
well mobilized, begin reconstruction. Typically, this begins with
creating the labial vestibular lining from superior to inferior and then
proceeding to the junction of the wet-dry vermilion with completion of
the remainder of the vermilion after the cutaneous portion of the lip is
completed.
- At this point, the
labial mucosa can be advanced as needed, with additional lengthening and
a back cut to allow for adequate eversion of the lip and to avoid a
tight-appearing lip postoperatively.
- Direct
attention to approximating the muscle bundles. Appropriately reorient
the nasolabial group of muscles toward the nasal spine. Follow this by
approximating the orbicularis, interdigitated with its opposing element
along the full length of the vertical lip. Inset the C flap to create a
symmetric columellar length and flare at its base. Millard originally
described the C flap to cross the nasal sill to insert into the lateral
lip element as a lateral rotation-advancement flap. Millard later
refined the C flap as a medial superior rotation flap to insert into the
medial lip element, augmenting the columellar height and creating a
more natural flare at the base of the medial footplate. The latter
method occasionally results in a nexus of scars at the base of the
columellar with unfavorable healing if the flaps are not well planned.
However, the authors and others continue to use the C flap in either
position as needed.
-

- Millard
repair. Two of the most common variations described with utilization of
the C Flap to correct the hemi-columellar deficiency (Millard II] and
the nasal sill alar base region [Millard I]
- Set
the ala base in place. As the C and A flaps and the ala are inset, take
care to leave an appropriate width to the nasal sill to avoid a
constricted-appearing nostril, which is nearly impossible to correct as a
secondary deformity.
- Approximate
the vermilion-cutaneous junction and inset the vermilion mucocutaneous
triangular flap. If the lip appears to be vertically short at this
point, the authors inset a small, 2- to 3-mm triangular flap into the
medial lip just above the vermilion.
- Use
dermal sutures to approximate the skin edges. Final approximation is
with either rapidly absorbing sutures or nylon sutures, ideally removed
at 5 days. If the cutaneous edges are well approximated with dermal
sutures alone, the authors occasionally use a cyanoacrylate-type
adhesive. Reposition the cleft alar cartilage with
suspension/transfixion sutures and a stent. Further shape the ala with
through-and-through absorbable sutures as needed.
Previous
Next Section: Preoperative Details
Postoperative Details
- Oral
feedings: For the child who is breastfed, the authors encourage
uninterrupted breastfeeding after surgery. Bottle-fed children can
resume feedings immediately following surgery with the same crosscut
nipple used before surgery. Some centers still advocate having the child
use a soft catheter-tip syringe for 10 days and then resuming normal
nipple bottle feeding, but the authors have found this degree of caution
to be unnecessary.
- Activities: The authors instruct
the parents to avoid giving the child pacifiers or toys with sharp
edges for 2 weeks after surgery. No other particular restrictions on
activity are necessary. Some centers do advocate the use of Velcro elbow
immobilizers on the patient for 10 days to minimize the risk of
inadvertent injury to the lip repair. These are periodically removed
several times a day under supervision.
- Lip care: The
exposed suture line at the base of the nose and red lip can be cleaned
using cotton swabs with diluted hydrogen peroxide, and topical
antibiotic ointment can be applied several times a day. The authors then
remove the permanent sutures on postoperative day 5-7. If cyanoacrylate
adhesive is used, no additional care is required in the immediate
postoperative period until the adhesive film comes off. The authors tell
the parents to expect noticeable scar contracture, erythema, and
firmness 4-6 weeks postsurgery, and that this gradually begins to
improve 6-12 months after the procedure. Typically, the authors instruct
parents to massage the upper lip during this phase and to avoid placing
the child in direct sunlight until the scar matures.
Previous
Next Section: Preoperative Details
Follow-upFollowing
cleft lip repair, patients are evaluated periodically by the various
cleft team members. Oral hygiene and dental care must be promoted,
hearing and speech must be assessed, and psychosocial evaluation and
treatment should be made available. Despite technical advances
and simultaneous correction of the nasal deformity performed at the time
of lip repair, a significant number of patients still require a
secondary procedure to restore nasal symmetry and improve function.
[10] Such
procedures should be individualized. The alar base symmetry is unlikely
to be improved until the alveolar alignment is corrected and grafted
with bone. The remaining components of cleft care are addressed in other
articles, including the following:
- Cleft Lip and Palate
- Cleft Palate
- Craniofacial, Bilateral Cleft Lip Repair
- Craniofacial, Bilateral Cleft Nasal Repair
- Craniofacial, Unilateral Cleft Nasal Repair
- Cleft Lip Nasal Deformity
Previous
Next Section: Preoperative Details
ComplicationsSeveral
common mistakes are made in the rotation-advancement method of
unilateral cleft lip repair. These include insufficient rotation of the R
flap, vermilion-cutaneous mismatch, vermilion notching and a
tight-appearing lateral lip element, a lateral muscle bulge, a laterally
displaced ala, and a constricted-appearing nostril. Aside from
unsatisfactory appearance of the surgical result, possible complications
include dehiscence of the repair (more common if the repair is delayed
until the child is learning to walk and falls) and excessive scar
formation and/or contracture of lip scars. If dehiscence occurs,
postpone re-operation until the induration has subsided completely. With
lip scars that appear red, thick, and contracted, the authors use an
occlusive tape dressing and if needed, Kenalog-10 (triamcinolone
acetonide) injection and/or flurandrenolide tape. For most repairs, the
observed contracture is part of the normal healing process and improves
with time. Postpone revisional surgery until the scar matures.
Intervention should be guided by the severity of the residual deformity.
Keep revisions to a minimum.
Previous
Next Section: Preoperative Details
Outcome and PrognosisCareful
preoperative assessment of the cleft lip deformity and attention to
detail in the reconstruction typically results in an excellent repair
that achieves many characteristics of the natural lip. Realistically,
many variables are involved beyond the technical aspects of a particular
repair. Ultimately, the outcome depends on the natural course of
uncomplicated healing of the initial repair, alignment of the skeletal
framework on which the lip rests, and the differential effect of normal
growth and development on the operated lip. While a poor initial
result is unlikely to improve with time, do not assume that an excellent
initial result will not require some revisional procedure because of
uncontrolled variables. Moreover, while the lip repair may be
acceptable, additional procedures required to achieve nasal symmetry are
not uncommon, despite the initial primary nasal surgery incorporated as
an integral part of lip repair.
Previous
Next Section: Preoperative Details
Future and ControversiesCleft
lip surgery has evolved from a geometrically defined "cookie-cutter"
type approach to a more adaptable repair using the principles outlined
by Millard's elegant rotation advancement technique.
[9, 11] Skin
flap design has led to a better understanding of the underlying
musculature that is disrupted by the cleft and the importance of
realignment of the individual bundles to create a functional repair.
With a better understanding of the underlying anatomy, cleft surgery
currently results in an excellent lip repair but is marred by a residual
cleft nasal deformity.Adjunct treatment. including early
presurgical alveolar and nasal molding with a palatal appliance. may
improve the long-term outcome, with the ultimate intent to remove the
accompanying cleft nasal deformity, which is the most common stigmata of
a facial cleft.Only close long-term follow-up care and an honest assessment of the results can establish these improvements in outcome.
[1] Advances
in the treatment of children with clefts will come only from a
team-based approach in which close cooperation of multiple disciplines
can address all the child's needs. Such children deserve to be cared for
at major centers where an interdisciplinary approach is possible and
substantial experience is available.
</li>



