Cognitive Lifestyle and Long-term Risk of Dementia and Survival After Diagnosis in a Multicenter Population-based CohortAbstract and Introduction AbstractAn active cognitive lifestyle has been linked to dementia incidence
and survival, but the separate and combined effects of its subcomponents
are not clear. Data were derived from the Medical Research Council
Cognitive Function and Ageing Study, a population-based study of 13,004
individuals in England and Wales first interviewed in 1991–1992 and
followed over a 10-year period for dementia incidence and 12 years for
mortality. A Cognitive Lifestyle Score (CLS), defined as a composite of
cognitive activity including education, occupational complexity, and
social engagement, was available for 12,600 individuals in 3 stages of
life. A higher CLS was protective of dementia (odds ratio = 0.6, 95%
confidence interval: 0.4, 0.9). Sensitivity analyses found this main
effect to be reliable and replicable even when considering just 2
components of the score, either education and occupation
or education and late-life social engagement. No single CLS factor was
associated with dementia incidence on its own. Survival differences did
not reach statistical significance. Our data suggest that more years of
education, as well as further stimulatory experiences in either midlife
or late life. are necessary for a protective link with dementia
incidence. There was little evidence of an effect of cognitive lifestyle
on survival after dementia diagnosis.
IntroductionEpidemiologic studies provide strong evidence linking an enriched
cognitive lifestyle with reduced dementia risk. For example, a
meta-analysis of 22 studies revealed a relative risk reduction for
incident dementia of 46% in those with more complex cognitive life
experiences (odds ratio (OR) = 0.54, 95% confidence interval (CI): 0.49,
0.59).
[1] Interestingly, despite differences in the way these factors have been
measured, the relative effects of high versus low education (OR = 0.53),
occupational complexity (OR = 0.56), and late-life leisure activities
(OR = 0.50), were highly consistent. Moreover, several more recent
prospective studies have revealed a dose-dependent association,
[2] whereby dementia risk declines with each step of increasing cognitively loaded leisure activities.
[3–6] What is not clear is the relative importance of the different cognitive
lifestyle components or their combinatorial interaction in relation to
dementia incidence or survival after diagnosis.
The Lifetime of Experiences Questionnaire (LEQ) was developed to
measure cognitive lifestyle differences between individuals by
integrating information on stimulatory educational, occupational, and
cognitively loaded leisure activities across the life span.
[7] Higher LEQ scores independently predict an attenuated rate of cognitive
decline over time, as well as a diminished rate of longitudinal
hippocampal atrophy.
[8] However, it is unclear whether this integrated approach to cognitive lifestyle can predict
incident dementia.
There are also no studies that we are aware of that have systematically
compared the impact of each of these components in isolation after
controlling for the other 2 factors or investigated whether a critical
pairwise combination of factors is as powerful as the triple
combination. Furthermore, the effects of cognitive lifestyle on survival
after diagnosis may dissociate from the protective effects against
dementia incidence, because higher education in those already with
dementia has been linked to increased mortality.
[9] Whether a similar pattern also holds for the other cognitive lifestyle
factors of occupational complexity and late-life cognitive activities is
unknown.
The issue of combined versus stand-alone effects of cognitive
lifestyle factors on both dementia incidence and then survival after
diagnosis has not been evaluated to date within the same
population-based longitudinal data set. The Medical Research Council
Cognitive Function and Ageing Study (CFAS) is a multicenter,
community-based, cohort study that has now been running for over 14
years and is well designed to address questions of this nature.
[10] Using a subset of questions derived from the LEQ covering the domains
of education, occupational complexity, and late-life cognitive
activities that were available as part of baseline and screening
questions from the Cognitive Function and Ageing Study, we were able to
evaluate the impact of cognitive lifestyle on both incident dementia and
survival time after diagnosis. This study therefore aimed at
investigating the individual and combined contribution of 3 major
cognitive lifestyle factors to incident dementia risk and survival after
diagnosis.
Materials and Methods Study Design and PopulationData are taken from the Cognitive Function and Ageing Study (http://www.cfas.ac.uk),
a large multicenter, population-based, prospective cohort study of
individuals aged 65 years or older in community and residential
settings. Full details are published elsewhere and briefly described
here.
[11, 12] Individuals were randomly selected from the Family Health Service
Authority lists in 5 areas of England and Wales, including 2 rural
(Cambridgeshire and Gwynedd) and 3 urban (Newcastle, Nottingham, and
Oxford). Baseline interviews were undertaken in 1991–1992. A 2-phase
screening procedure was used. At baseline screening, 13,004 individuals
provided information on physical, behavioral, and sociodemographic
status in addition to aspects of health, including self-reported chronic
conditions, and cognition using the Mini-Mental State Examination
(MMSE)
[13] and selected items from the Geriatric Mental State-Automated Geriatric Examination for Computer Assisted Taxonomy (AGECAT).
[14] Following the baseline interview, a subsample of approximately 20% (
n = 2,640) were selected on the basis of age, center, and cognitive
ability and weighted toward the cognitively frail, to participate in a
more detailed assessment interview that included the full measures of
mood and organicity of the AGECAT
[15] and so allowed dementia diagnosis. At 2 years, those who had not
undertaken an assessment interview were rescreened with a further 20%
undergoing the diagnostic interview. Respondents who underwent further
assessment at baseline were asked to complete 1 or 2 yearly follow-up
interviews including a diagnostic interview.
[12] Further interviews were undertaken at 3, 6, 8, and 10 years (different
subgroups targeted at each time with a maximum of 8 interviews in 10
years). At each diagnostic interview depression, anxiety, and dementia
status were derived from the full AGECAT diagnostic algorithm. Dementia
was defined as an AGECAT organicity rating case level of 3 or above and
is comparable to dementia as diagnosed by the
Diagnostic and Statistical Manual of Mental Disorders: DSM-IIIR.
[14, 15] Depression and anxiety were both defined as an AGECAT symptom level of 3
or above. Informant interviews were undertaken on those with the
detailed assessment interviews and from which the Blessed Dementia
Rating Scale can be measured. Incident dementia was measured for all
individuals who developed dementia at follow-up who did not have
dementia at the previous interview.
[16] A history of vascular risk factors (diabetes, medicated high blood
pressure, heart attack, angina, stroke) was asked at each interview, as
well as smoking history at baseline. These factors were combined to
produce a vascular risk factor score: Individuals were given 1 point for
the presence of each risk factor, except for smoking where individuals
were coded as 0 for nonsmokers, 1 for former smokers (more than 5 years
ago), and 2 for current smokers. Individuals could therefore score
between 0 and 8, and the median score was 2. Data from all waves have
been used in the analysis (Data Version 8.2, December 2006), in addition
to death notifications from the United Kingdom's National Health
Service Central Register.
This study had ethical approval from the Eastern Anglia Multicentre
Research Ethics Committee and all local ethical committees for the
duration of the study (1990 to date). All individuals gave written,
informed consent.
Cognitive Lifestyle ScoreThe LEQ asks detailed information about an individual's range and
intensity of educational, occupational, and cognitive lifestyle
activities in all 3 phases of life (young adulthood, midlife, and late
life).
[7] The original Cognitive Function and Ageing Study protocol did not cover
these domains in as much detail as the LEQ, so we constructed a
simplified proxy for the LEQ called the Cognitive Lifestyle Score (CLS)
as follows. Matches were found between the study's baseline/screening
questions and LEQ questions, and the resultant abbreviated score was
tested to determine if it correlated sufficiently highly with the
overall LEQ. This test was completed by using data from the LEQ
validation study.
[7] The following combination of questions was found to correlate significantly with the total LEQ score (
r = 0.60,
P < 0.0001,
n = 70; data not shown):
- Educational level in young adulthood: assessed by the self-report question, "how many years of full-time education?"
- Occupational complexity in midlife:
assessed by recording the participant's main occupation in terms of
years most worked and then recoding it using 2 systems, his/her social
class grouping (from I to VI) and socioeconomic grouping (from 11 to
150). These 2 systems distinguish different occupations by complexity
and status.[17]
Social class groupings were exploded with the socioeconomic groupings
and ranked to create a finer detail than either grouping alone. These
groups have then been reclassified into 14 groups, the 15th representing
housewives who do not have a formal code within the United Kingdom
system (n = 2,171 women). These scores were reversed so as to
be in the same direction as education and current social engagement
(with low scores indicating less cognitive lifestyle activity).
- Social engagement (current levels in
later life): calculated on the basis of three 3-point Likert scale
questions (i.e,, minimum of 3 and maximum of 9): a) frequency of contact
with children and other relatives; b) frequency of face-to-face contact
with neighbors; and c) frequency of attending meetings, clubs, and
other social events.
To enable each subscore to have an equal and unbiased contribution to
the combined score, the CLS was generated by using a weighted function
prior to any risk factor analysis:

Weighting factors for each component were empirically derived at the
whole-group level so that the resultant weighted mean scores for each
component were equivalent. This method follows the structure of the LEQ,
whereby young adulthood, midlife, and late-life subscores are also
equally weighted. Housewives were given an occupation of minimum
complexity. Following common practice, sex-specific tertiles for the CLS
were generated to investigate contrasting high, medium, and low
cognitive lifestyle groups. The associations among the 3 CLS subscores
were compared by using Spearman's rank correlation coefficient.
Statistical Methods Dementia Incidence. A nested
case-control analysis of incident dementia versus nondementia has been
undertaken adjusting for study design, attrition, age at interview, and
wave of interview. The nested case-control approach considers each wave
of follow-up separately and defines cases and controls for that time
point. Cases are therefore compared with the controls nested at the same
follow-up time. Multivariable logistic regression analyses have been
used.
Dementia Survival. Median survival
times by group and Cox proportional hazards regression have been used to
investigate differences in survival for incident dementia cases.
Proportional hazards assumptions have been checked by using Schoenfield
residuals. Deaths to the end of 2008 were included in this analysis.
Results Study PopulationThe study consists of 13,004 individuals aged 65 years or above with
baseline interview. There are 7,847 women and 5,157 men; 1,682 of 12,747
(13%) had a Mini-Mental State Examination score of <22 at baseline
interview. Individuals were followed from baseline by using interviews
at 0, 2, 6, and 10 years (mean length of time on active follow-up: 4.1
years for the 11,591 who survived to the follow-up interview).
Cognitive Lifestyle ScoreThe continuous CLS measure was generated for 12,600 individuals
(97%), with 157 missing education components, 320 missing occupation
components, and 83 missing current activity components. Of the 404
individuals with missing data, 99 could be classified within the
sex-specific tertiles regardless of their missing information as their
grouping did not change after replacement with the maximum or minimum
possible value, thereby leaving 12,699 individuals for analysis of
tertile groups. Figure 1 shows the distribution of the CLS that
approximated a normal distribution with slight right-hand skewness. The
CLS had a mean of 41.2 and a standard deviation of 11.2.
Table 1 also shows the general characteristics of the sample.

(Enlarge Image)
|
Figure 1.
Distribution of the Cognitive Lifestyle Score (n = 12,699) in the Cognitive Function and Ageing Study Sample, England and Wales, 1991–2006.
|
<blockquote>

</blockquote>
Figure 1.
Distribution of the Cognitive Lifestyle Score (
n = 12,699) in the Cognitive Function and Ageing Study Sample, England and Wales, 1991–2006.
Incident DementiaDuring the course of the longitudinal phase of the study, there have been 438 incident dementia cases.
[16] Of these, 361 were diagnosed at interviews where a nested case-control
study could be undertaken (120 cases at year 2, 138 at year 6, and 103
at year 10). The other cases were diagnosed at annual follow-up points
between interviews where control status is not known for all
individuals. These 361 individuals were compared with those individuals
who did not develop dementia.
As shown in
Table 2,
higher scores on the total CLS appear to be protective against the
incidence of dementia, with a significant reduction in relative risk for
the high LEQ group compared with the low LEQ group. Controlling for the
covariates of age, sex, wave, and vascular risk factors did not
eliminate this association (OR = 0.6, 95% CI: 0.4, 0.9). We also
analyzed each CLS component's prediction of incident dementia, before
and after adjusting for the other CLS components. No particular
component reached statistical significance (for all levels,
P > 0.2, except for enriched occupational complexity,
P = 0.07). In general, each of the 3 subcomponents of the CLS was only weakly correlated with each of the others (
Table 3).
We additionally tested the 3 different possible pairwise combinations
of CLS components after controlling for the remaining single CLS factor
(
Table 2). High levels of education plus occupational complexity
or of education plus late life social engagement appeared to confer risk
similar to that of the complete combination (OR = 0.6 for both). The
combination of enriched occupational complexity and late life social
engagement was not significantly associated with a change in dementia
incidence after taking educational level into account. Figure 2 shows
how different combinations of CLS components were associated with
dementia risk and combined to produce an overall risk.
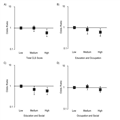
(Enlarge Image)
|
Figure 2.
Adjusted odds ratios for incident dementia in individuals with low
(reference), medium, and high cognitive lifestyle in the Cognitive
Function and Ageing Study Sample, England and Wales, 1991–2006. All
graphs show point estimates as well as 95% confidence intervals after
controlling for background variables of age, sex, interview wave, and a
combination of vascular risk factors. Risk estimates have been based on
complete Cognitive Lifestyle Score (CLS) (A), combined education and
occupational factors (controlling in addition for social engagement)
(B), education and social engagement (controlling for occupational
factors) (C), and occupational and social engagement factors
(controlling for education) (D).
|
<blockquote>

</blockquote>
Figure 2.
Adjusted odds ratios for incident dementia in
individuals with low (reference), medium, and high cognitive lifestyle
in the Cognitive Function and Ageing Study Sample, England and Wales,
1991–2006. All graphs show point estimates as well as 95% confidence
intervals after controlling for background variables of age, sex,
interview wave, and a combination of vascular risk factors. Risk
estimates have been based on complete Cognitive Lifestyle Score (CLS)
(A), combined education and occupational factors (controlling in
addition for social engagement) (B), education and social engagement
(controlling for occupational factors) (C), and occupational and social
engagement factors (controlling for education) (D).
Sensitivity AnalysisSensitivity analyses were carried out to determine whether other
potential factors moderated our key finding of decreased dementia risk
in the high CLS group. These factors included time to diagnosis,
removing individuals who became demented in the first 2 years of
follow-up, splitting our summary vascular risk score into scores for
individual cardiovascular risk factors, history of head injury or
boxing, and comorbid depression or other emotional problems. As can be
seen in
Table 4, none of these factors significantly altered our key findings.
Because preclinical and undiagnosed dementia may have affected our
estimation of the risk of social engagement on dementia incidence more
than the other CLS components, we also tested this relation before and
after excluding individuals who became demented within the first 2 years
of follow-up. Again, the effects were minimal, with odds ratios for
high social engagement compared with low changing from 0.71 to 0.69,
respectively.
SurvivalOf the 438 incident dementia respondents with survival data, there
are 434 (99%) that have a CLS. Of these, 398 (92%) had died by December
31, 2008, with a median survival time of 4.5 years (interquartile range:
2.8–6.9). There was no positive evidence that individuals with
contrasting CLS scores differed in terms of age at dementia onset or
survival time after diagnosis (
Table 5).
Some evidence of survival differences was shown for 2 comparisons,
although larger numbers are needed to confirm these findings. The medium
and high CLS groups had an adjusted hazard ratio of 1.3 (95% CI: 1.0,
1.7) for decreased survival time compared with the low CLS group;
similarly, those with a high occupational complexity had decreased
survival time (hazard ratio = 1.4, 95% CI: 1.0, 1.9). No interactions
were found between the CLS and severity (for both the Blessed Dementia
Rating Scale and the Mini-Mental State Examination:
P > 0.2).
DiscussionFourteen-year prospective data from a large, multicenter, and
community-based study in the United Kingdom were used to evaluate the
combined and independent associatons of cognitive lifestyle on ongoing
dementia risk and survival. We found that the combination of education,
occupational complexity, and late-life social engagement, rather than
any individual component, was an independent predictor of dementia risk.
Those with a higher overall CLS were at 40% decreased risk for
developing dementia. There was no clear association between cognitive
lifestyle and survival time after diagnosis.
Our findings are consistent with previous epidemiologic estimates of
the protective effects of cognitive lifestyle. For example, our
meta-analysis of cognitive lifestyle found an overall relative risk
reduction of dementia incidence of 46%,
[1] comparable to 40% in this study. Although reverse causality cannot be
completely accounted for, our results are unlikely to be influenced by a
diagnostic threshold effect, because including time to diagnosis as a
covariate or excluding those individuals who became demented within 2
years of baseline interview did not substantively change our results.
Furthermore, exclusion of individuals who became demented within 2 years
of follow-up did not alter the estimated protective association of high
late-life social engagement, the CLS factor most vulnerable to reserve
causality bias if present. These analyses also found no moderating
influence of depression, head injury, or the use of individual
cardiovascular risk factors rather than a vascular summary score in our
models. On the basis of our 10-year population-based longitudinal study,
an active cognitive lifestyle therefore appears to reliably predict
lower dementia risk.
Each of the CLS subcomponents measured relatively independent facets
of cognitive lifestyle because they were only weakly intercorrelated. It
is therefore interesting that no particular single cognitive lifestyle
component was significantly associated with dementia risk, either before
or after adjusting for the other 2 components. Cohort studies of
occupational complexity that have simultaneously controlled for
education have produced conflicting results; some have noted a residual
protective effect on incident dementia,
[18] while others have not.
[5, 19, 20] Only 1 previous study that controlled for education and occupation when
examining late-life leisure activities found a signification protective
effect.
[21] Perhaps more importantly, our systematic review suggested that the
overall cohort event rate is a key consideration when testing for the
differential effects of a cognitive lifestyle factor on dementia
incidence.
[1] In the current study, 434 incident dementia cases in the subsample from
the baseline cohort of 12,699 were followed over a 10-year period.
After accounting for study design, this averages to a new-case rate of
1.8% per year.
[10] In our meta-analysis, dementia event rates ranged from 0.2% to 4.9% per
annum. Hence, the midrange event rate observed in the Cognitive
Function and Ageing Study may explain why individual CLS factors did not
reach significance. Even large cohort studies may be insufficiently
powered to fully analyze interactions among individual cognitive
lifestyle components, a task that may require meta-analyses
incorporating individual patient data, background variables, and study
design.
By contrast, paired combinations of cognitive lifestyle components
were also tested while controlling for the third factor, yielding a
different pattern. When a high level of education was combined with
either a complex occupation or social engagement in later life, a
significant 40% level of risk reduction was found (Figure 2, B and C).
Alternatively, a complex job plus late-life social engagement was not
sufficient to reduce incident dementia risk after adjusting for
education (Figure 2D). Particular combinations of CLS factors therefore
appear to be more strongly predictive of reduced dementia risk than
others or when considered in isolation. Specifically, a higher level of
education may be most effective in providing some protection against
dementia when in combination with subsequent cognitive complexity and
stimulation in later life.
There was no compelling evidence that an enriched cognitive lifestyle is linked to decreased survival. Stern et al.
[22] found that those with increased cognitive reserve in the form of higher
education or occupational complexity experienced accelerated cognitive
decline. Although this relation has been replicated in some cohort
studies,
[23–25] others have found either no link
[26, 27] or even the opposite finding.
[28] The reasons for these discrepancies may include the selection of
cognitive outcome measure, various degrees of dementia severity,
different follow-up time periods, or an interaction with comorbid
depression.
[29] Importantly, in this study we did not specifically examine the rate
of cognitive decline after diagnosis but rather survival time, and these
variables may not necessarily be correlated. Although individuals with
high educational levels experienced faster cognitive decline after
diagnosis on the basis of repeated Mini-Mental State Examination tests,
Bruandet et al.
[30] found there was no effect on time to death. Generally, study results of
differential survival after diagnosis based on educational level have
not been consistent, including positive
[9, 31] and negative
[18, 32, 33] studies. As identified in our meta-analysis, predictions based on
educational levels exhibit a significant degree of heterogeneity,
[1] so the overall educational level of the cohort may be important. In our
study, individuals with a very low level of education were not seen,
reflecting its rare occurrence in the population of England and Wales.
Most individuals, for example, had 9 years of full-time education, with
very few having less than 8 years. Because individuals with higher
levels of education may mask their dementia and falsely achieve a higher
score, our study benefited from selecting individuals for an initial
diagnostic interview on the basis of 2 separate screening mechanisms.
The potential for diagnostic bias was thereby reduced as the result of a
more random sampling of the complete population.
Other important factors that may have contributed to our null
dementia survival findings include the level of medical comorbidity in
the sample, overall disease severity, and the length of follow-up.
Despite these issues, we noted near-significant findings in the
direction of abbreviated survival time in the higher cognitive lifestyle
group. The effect may therefore be subtle and require either a larger
sample size for detection or the use of more complex longitudinal
modeling to dissociate the effects on time of presentation versus the
rate of progression and time to death. These are interesting theoretical
questions for future research.
There were also some limitations to this study. The information used
to generate the CLS was limited to those questions originally devised by
the Cognitive Function and Ageing Study team over 14 years ago and, for
this reason, the full range of cognitive lifestyle activities was not
assessed. Assessment of social engagement, for example, was particularly
simplistic in comparison to current methods. The CLS also uses
information from the baseline interview, and this may introduce bias, as
engagement in cognitive leisure activities will almost certainly be
different for the young-old than for the oldest old. Furthermore, our
component scores assume a static level of participation, whereas
individuals' educational, occupational complexity, and cognitive
lifestyle activities may change over time. A more detailed assessment,
using for example the
Lifetime of Experiences Questionnaire [7] in a longitudinal setting, could therefore be more informative.
Finally, many women in this generation were not employed while married.
It is standard practice in the United Kingdom for married and widowed
women to be classified according to their husband's occupation for
social class, while here these individuals' occupations were coded as
housewives. Future studies could therefore focus on whether married
women who did not participate in the workforce have differential
dementia risk based on their husbands' cognitive lifestyles.
In conclusion, we compared dementia risk and survival in individuals
with a range of cognitive lifestyle patterns using the Cognitive
Function and Ageing Study longitudinal data set. Our main finding was a
40% reduced risk for developing dementia in those that maintain a high
level of cognitive complexity throughout their lives, independent of
other known risk factors. By comparison, individual components of an
active cognitive lifestyle, such as educational achievement,
occupational complexity, or social engagement, were not linked to a
protective effect. The 2-factor combination of higher education and
either a more complex occupation or late-life social engagement was as
effective in reducing dementia risk as the complete 3-factor
combination. Some level of cognitive enrichment beyond education in
young adulthood may therefore be required for more effective dementia
prevention. No conclusive evidence was found for an effect on survival
time after diagnosis, yet this may be due to a relatively subtle
relation that requires more investigation.



