Contact Lens Complications
Introduction Contact lens–related complications range from self-limiting to sight
threatening, which require rapid diagnosis and treatment to prevent
vision loss. With millions of individuals wearing contact lenses, even a
small percentage of complications can constitute a major public health
problem. Contact lens complications are as varied as they are common,
involving the lids, conjunctiva, and all layers of the cornea (ie,
epithelium, stroma, endothelium). When reviewing complications, grouping
them according to which anatomical structure is primarily affected can
be helpful.
For illustrated demonstrations of removing different types of contact lenses, see eMedicine's Contact Lens Removal article.
Lids Giant papillary conjunctivitis is a common complication among soft contact lens wearers.
1 This complication is often addressed by changing 1 of the following 3 factors:
- Increasing the frequency of lens disposal
- Decreasing the length of contact lens wear
- Switching to a stronger cleaning solution
Rarely, rigid contact lenses can dislocate from the cornea and
settle into the upper fornix. If undetected, the lens may erode through
the conjunctiva and enter the soft tissues of the lid, where it can
remain relatively asymptomatic. Alternatively, the tissues around the
contact lens can become irritated and inflamed, producing a sterile
abscess. The lens foreign body can incite the formulation of
granulation tissue around the lens, encapsulating it in a cystlike
structure.
A mechanical ptosis
is occasionally the result of the mass of lens, scar, and fibrous
tissue in the lid. An embedded contact lens also can produce enough
scarring and contraction of the lid tissues to produce a lid retraction.
The contact lens need not migrate into the lid tissues to produce
ptosis. A ptotic lid can result simply from severe giant papillary
conjunctivitis (GPC).
Occasionally, ptosis can be seen in contact lens wearers without any
inflammation, lens migration, or other definite cause. Hard contact
lens wearers may develop ptosis from levator aponeurosis disinsertion
from years of repeated stretching of the lid during lens removal. A
second proposed mechanism is that the repeated trauma of the lens edge
rubbing against the palpebral conjunctiva produces chronic inflammation
and edema in the soft tissues of the lid. Because all or part of the
ptosis may resolve with discontinuation of contact lens wear, it is
recommended that patients stop wearing their lenses for a period of
time prior to surgical correction of the ptosis.
Tear Film The tear film provides a smooth and transparent refractive surface,
essential moisture, and oxygen to the epithelial cells. Tears also
contain immunoglobulins, complement, and other proteins, which help
protect against infection. The health of the ocular surface is entirely
dependent upon an adequate quantity and quality of tear film, both of
which can be altered by the presence of contact lenses.
Bacteria and debris are collected in the tear film, wiped by the lid
blink, and rinsed away from the surface of the eye. The presence of a
contact lens on the eye substantially reduces the interchange of tears
across the ocular surface. Rigid lenses reduce the tear exchange
compared to no contact lens wear. Soft lenses reduce the tear exchange
to an even greater extent and the larger the diameter, the greater the
reduction.
The effect of contact lenses on the tear film can vary from one part of
the cornea to another part of the cornea. Tear film instability exists
in the interpalpebral fissure in the periphery of the cornea, the
so-called 3- and 9-o'clock areas, in wearers of rigid contact lenses. A
rigid lens that is fit poorly often produces corneal staining at these
sites. Epithelial damage in these areas is associated with instability
and abnormalities in the mucin layer of the tear film.
In addition to the mixing of tears, the content of the tears can be
altered by the presence of contact lenses. Overnight wear increases the
levels of tear proteins compared to daily wear or no wear of contact
lenses.
Conjunctiva Conjunctival Abnormalities Contact allergyA contact dermatitis hypersensitivity reaction can be produced by one
of a host of chemicals, which are found in contact lens solutions. A
typical reaction consists of marked itching with varying amounts of
injection, burning, redness, tearing, mucoid discharge, and
occasionally chemosis. In addition, the lid may become edematous and
erythematous. Cold compresses and the elimination of the offending
chemical usually relieves symptoms. A short course of topical steroids
can be used in particularly severe instances.
Giant papillary conjunctivitisApproximately 1-3% of contact lens wearers eventually develop a symptom
complex of GPC consisting of conjunctival injection, mucoid discharge,
itching, tear film debris, coated lenses, blurred vision, excess lens
movement, and blurred vision. These symptoms may remain minimal or
progress to complete lens intolerance. The tarsal conjunctiva becomes
inflamed and hypertrophied. This inflammatory hypertrophy is
morphologically similar to the papillary hypertrophy of vernal
conjunctivitis.
The etiology of GPC is multifactorial and begins with the formation of
deposits on the surface of the lens. The constant trauma of the
blinking lid rubbing on the surface of the lens exposes the deposits to
the conjunctival lymphatic system. The antigens associated with the
deposits incite an immune response in the conjunctiva. This condition
can occur whenever a foreign substance chronically rubs the tarsal
conjunctiva, such as ocular prostheses, exposed scleral buckles, nylon
sutures, and gas-permeable contact lenses but most commonly is
associated with soft contact lenses.
Typically, papillae (0.3 mm or larger) are seen surrounded by thickened
and hypervascular conjunctiva. The hyperplastic epithelium extends
down into the underlying stoma. The epithelium is infiltrated with mast
cells, and the stroma is infiltrated with basophils and eosinophils.
The symptoms of GPC are exacerbated by anything that increases the
contact of the lens deposits with the tarsal conjunctiva, such as
increased numbers of deposits, increased size of the contact lens, and
increased wearing time, especially overnight wear.
Treatment of GPC consists of reducing the amount of contact between the
deposits and the conjunctiva. Frequent enzymatic cleaning of the
contact lenses, frequent replacement of contact lenses (disposable
lenses), reduction in wearing time, and the use of lenses that resist
deposit formation are effective treatments.
Medications that suppress the immune response also can be used. Topical
steroids also reduce symptoms; however, the risk of complications
limits their use. Topical mast cell stabilizers, such as 4% cromolyn,
have some effectiveness in reducing the symptoms of GPC. Medical
treatments generally are used for a short duration in acute
exacerbations. The most effective treatment usually is reduced wearing
time and switching to disposable contact lenses.
Contact lens–induced superior limbic keratoconjunctivitisContact lens–induced superior limbic keratoconjunctivitis
(CL-SLK) is an immunologic reaction in the peripheral conjunctiva
produced by contact lens wear that is similar to that seen in Theodore
superior limbic keratoconjunctivitis (SLK). It is characterized by
conjunctival thickening, erythema, and a variable amount of fluorescein
staining of the superior bulbar conjunctiva.
The keratinized epithelium loses many of its goblet cells and is
invaded by neutrophils. Foreign body sensation, photophobia, tearing,
burning, occasional itching, and reduced visual acuity due to punctate
epitheliopathy are typical symptoms of CL-SLK.
Although similar in name, CL-SLK is a separate and distinct entity from
Theodore SLK. CL-SLK can be differentiated by a lack of filaments,
minimal tarsal papillary reaction, impaired vision, and lack of
association with thyroid disease. It also is not limited to the
superior conjunctiva but can be circumferential.
CL-SLK may be caused by excessive lens movement or sensitivity to
thimerosal. Treatment consists of discontinuing contact lens wear until
the epithelium returns to normal and the symptoms resolve. Refitting
with better fitting lenses, using preservative-free solutions with a
hydrogen peroxide disinfecting system, or switching to rigid
gas-permeable (RGP) contact lenses may permit a resumption of contact
lens wear
=================================
Automatic Contact Lens Cleaner System


 READ MORE...CLICK HEREGET IT HERE
READ MORE...CLICK HEREGET IT HERE
save 30% order now
===================
Related Subject ABC of Eyes (ABC Series)Becker-Shaffer's Diagnosis and Therapy of the GlaucomasBorish's Clinical Refraction (Benjamin, Borish's Clinical Refraction) Ophthalmology Atlas Test Yourself Atlas in OphthalmologyPearls of Glaucoma Management - Feb 2010 Edition 







































 Stromal scar and corneal neovascularization.
Stromal scar and corneal neovascularization. </blockquote>Stromal scar and corneal neovascularization
</blockquote>Stromal scar and corneal neovascularization Close-up view of stromal scar and corneal neovascularization.
Close-up view of stromal scar and corneal neovascularization.

 Acanthamoeba infection.
Acanthamoeba infection. </blockquote>Acanthamoeba infection.
</blockquote>Acanthamoeba infection.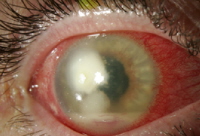 Acanthamoeba infection.
Acanthamoeba infection. </blockquote>Acanthamoeba infection.
</blockquote>Acanthamoeba infection. Corneal transplant following acanthamoeba infection.
Corneal transplant following acanthamoeba infection. </blockquote>Corneal transplant following acanthamoeba infection.
</blockquote>Corneal transplant following acanthamoeba infection.